A Tale of Resilience: Suresh's Extraordinary Road to Recovery
Meet Mr. Suresh, a 27-year-old construction site supervisor with an inspiring story of overcoming adversity. Suresh's journey began when he arrived at the Emergency Department, his body burdened with abdominal distension, vomiting, and constipation. These symptoms had plagued him for three days, during which he sought treatment at two different hospitals, but his condition only deteriorated. Recognizing the gravity of the situation, he was referred to Believers Church Medical College Hospital (BCMCH).
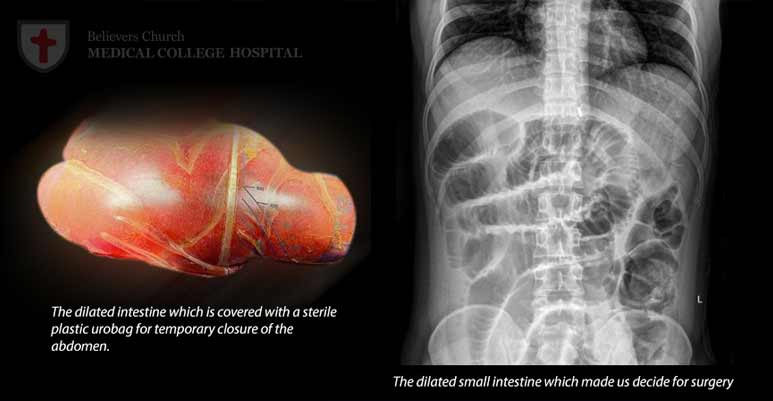
The emergency physician swiftly identified the critical nature of Suresh's condition—intestinal obstruction and sepsis, a potentially life-threatening bloodstream infection. Suresh's kidneys were severely compromised, and his white blood cell count indicated a dire septic state. An abdominal X-ray confirmed the intestinal obstruction. The surgical team, cognizant of the medical and surgical emergency at hand, discussed the urgency of surgery with Suresh's family and initiated resuscitation, swiftly wheeling him into the operating room that very night.
In the operating room, surgeons uncovered a congenital anomaly responsible for the intestinal obstruction. While correctable, the procedure revealed that closing the abdomen posed a significant challenge due to the bowel loops' distension and oedema. Closing under tension would be perilous and detrimental to his kidney function. Thus, a temporary solution was implemented—a sterile cover known as a laparotomy procedure, using readily available materials like a urobag. This damage control surgery approach allowed monitoring in the ICU.
Suresh, at first on a ventilator, faced the challenge of adapting to life with part of his intestines in the urobag. However, the critical care consultants and nursing staff rose to the occasion. Two days later, Suresh underwent a second surgery, which removed the urobag, emptied the bowels, and closed the skin. Post-surgery, he returned to the ICU. Although his condition briefly deteriorated, marked by a drop in haemoglobin levels, Suresh's youth and resilient spirit played in his favour. His positive outlook, coupled with cooperation in respiratory exercises and physiotherapy despite pain and discomfort, boosted his recovery. Remarkably, his kidney function improved without requiring dialysis.
During this period, Suresh had to be kept fasting due to his distended abdomen's inability to process normal food, leading to weakness. Blood transfusions and Total Parenteral Nutrition (TPN) were initiated. His nutritional needs were met through round-the-clock care, and he gradually improved. After almost two weeks from his first surgery, he began an oral diet and was eventually moved to the ward.
However, a wound infection, a not uncommon complication following bowel surgery in critically ill patients, arose. To manage this, Negative Pressure Wound Therapy (NPWT) was applied, aided by antibiotics. NPWT, a technique that promotes wound healing, was instrumental in controlling the infection and facilitating normal wound healing. Suresh's first steps following this ordeal filled him with much-needed hope for the future.
Suresh recently had his first post-discharge review in the Surgery OPD and is on the path to recovery. His abdominal wound is expected to heal in a few more weeks, after which he can return to work and resume a normal life. We extend our sincere thanks to the dedicated teams in the Emergency Department, Operation Theatre, Anaesthesiology, Intensive Care Unit, Cardiology, and Surgery at BCMCH. Their quick thinking and compassionate care exemplify the hospital's commitment to excellence. We are equally grateful to Suresh's family for their trust, support, and encouragement throughout his journey to recovery.
(To protect patient confidentiality, the patient's name has been changed.)
Other Stories
-

A Miracle of Survival: Overcoming Aortoesophageal…
A 5-year-old boy arrived at our Emergency Room on the night of April 19th, after experiencing two episodes of hematemesis…
-

An Inspiring Patient Testimonial: Believers Church…
I am writing to share my family's deeply heartfelt experience at Believers Church Medical College Hospital. In January 2021, my…
-

Heartfelt Appreciation for Exceptional Care
I would like to express my heartfelt gratitude to the entire ICU team at your facility, with special mention to…
Read more